
Expect Remarkable for You and Your Family.
Your journey to better health starts here. Schedule online to connect with a primary care doctor who is here for you every step of the way.
Care when and where you need it
Same & next-day sick visits
- Convenient access to the right providers and facilities
- Same & next-day appointments and online scheduling for illness or injury
Virtual care
- 24/7 on-demand video visits for new and existing patients
- Schedule a video visit with your preferred provider, where available
Urgent & walk-in care
- Convenient walk-in care to meet your non-emergency needs
- Quick access to care for common health problems
Emergency care
- Immediate care from an extensive network of specialists
- Emergency rooms and medical centers available 24/7

Remarkable careers start here.
Be part of our incredible team, helping us create a healthier future and bring remarkable experiences to life.
We're hiring for all positions, including physicians, advanced practice providers, registered nurses, radiology technologists, medical assistants and pharmacy techs. Check out our exciting opportunities and apply to join our team today.
Find Your Career
Elevate your nursing career.
RNs, you can earn up to a $30,000 signing bonus and up to a $7,500 relocation package when you join Novant Health. Even more roles now qualify.
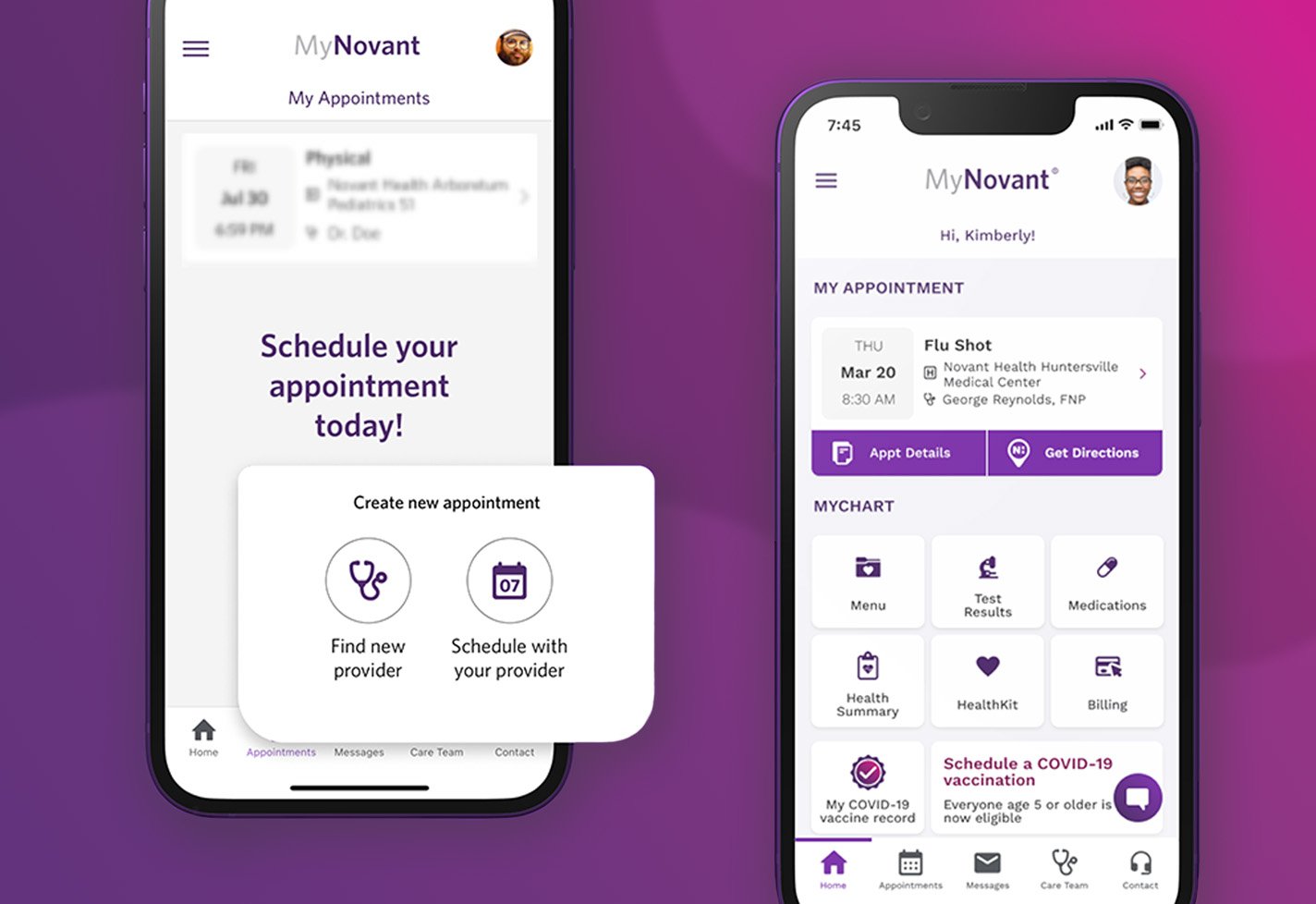
MyNovant portal
It's your health, in your hands.
Access and manage all your health information in one place with the MyChart app. Sign in to your MyChart account to schedule and see appointments, conduct virtual visits, message your doctor, view health records and more.
Sign In to MyNovant